Wider testing urged for ‘bad cholesterol’ linked to heart attacks in younger people
Doctors are calling for more testing for a marker of “bad cholesterol” that can cause sudden heart attacks in younger people and could be elevated in more than 5 million Australians.
Professor Jason Kovacic, executive director of the Victor Chang Cardiac Research Institute in Sydney, said there was a huge amount of data “unquestionably” linking higher levels of a little-known cholesterol – lipoprotein(a), or Lp(a) – to strokes and heart attacks.
Professor Jason Kovacic, executive director of the Victor Chang Cardiac Research Institute.
Kovacic said up to 20 per cent of the population might have at least a mild elevation of Lp(a), but many doctors and the wider public were unaware of what he called the “second bad cholesterol”.
Unlike the other type of bad cholesterol, LDL, Lp(a) is mostly linked to genetics rather than lifestyle factors.
Cardiologists have been finding elevated levels of Lp(a) among families with a history of heart attacks or people who had heart attacks and strokes in their 30s.
Kovacic said Lp(a) was made up of particles that carry cholesterol around the body. It is known to be a major risk factor for atherosclerosis, which is hardening and narrowing of the arteries.
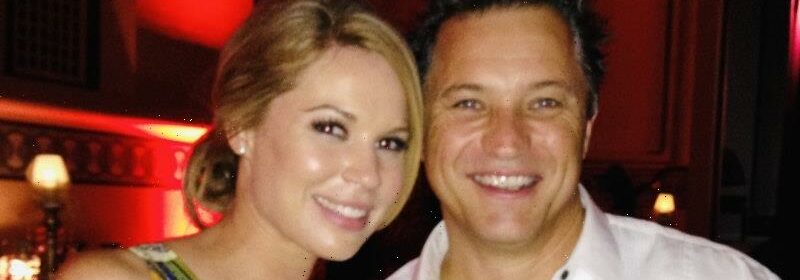
Ben Beale, seen here with wife Sarah, died of a heart attack at 47 while jogging.
“We have long wondered why healthy people with low cholesterol levels and seemingly no other major risk factors like smoking or diabetes can suffer heart attacks,” he said. “But we now understand that high levels of Lp(a) could be responsible for many of these events.”
Sarah Beale said she was told her husband, Ben, had suffered a one-off catastrophic event when he died of a heart attack at 47 while out jogging in Perth in 2017.
But Beale said it never sat right with her. The popular and energetic executive had been training for a charity boxing match and eating well. And before his death, the father of five was tested, showing a low chance of having a heart attack in the future.
However, Kovacic said an autopsy revealed Ben had extensive cholesterol and fat in the walls of his arteries.
Ben Beale with his children Jasmin, Mitch, Hayden and Jett.
“That’s what we see in people that have genetically higher levels of Lp(a) … they just have rapid progression of a lot of cholesterol and fat laid out in the walls of their arteries, and they just have a heart attack early on before the things even had an opportunity to harden [into calcium],” the cardiologist said.
Beale said she felt the medical system failed her husband, who had been to a doctor five times before his heart attack complaining of symptoms. She said the autopsy showed he had suffered two or three heart attacks previously, and that a portion of his heart was already dead.
“He consistently got told to lose weight, to get fitter. But he was extremely fit. He had a calcium score of zero. In reality, they should have had more blood tests done. If we’d known, he could have been tested for Lp(a). It would have completely changed our entire life,” she said.
Beale said four family members had since been identified with elevated Lp(a) and Ben’s older children had been tested and cleared.
“It’s high time that this test becomes mainstream, so we can protect other families from losing their loved ones,” she said.
Associate Professor Peter Psaltis, who leads the heart and vascular program at the South Australian Health and Medical Research Institute, said he would like to see improved testing for Lp(a) for those at higher risk.
That would include people who had developed heart disease before the age of 65, people who have had multiple heart attacks or strokes despite treatment and those with a strong family history of early heart disease.
But Psaltis said many cardiologists still did not know when to test for Lp(a) and there was no Medicare rebate for the test, which costs patients up to $40. He said it should be covered by Medicare for those at risk, particularly as it only needed to be done once in a person’s life.
Heightened Lp(a) levels remain challenging to treat, but new therapies to lower Lp(a) could be a few years away, and Kovacic said that in the interim there were other things specialists could do to help manage the condition.
If the new treatments in clinical studies proved successful at reducing heart attacks and strokes, it would bolster the case for universal screening of all Australians.
“There are some groups already advocating for this to be a test that everyone gets at least once in their lifetime,” Kovacic said.
The Morning Edition newsletter is our guide to the day’s most important and interesting stories, analysis and insights. Sign up here.
Most Viewed in National
From our partners
Source: Read Full Article


