The great diabetes divide playing out across Melbourne
Save articles for later
Add articles to your saved list and come back to them any time.
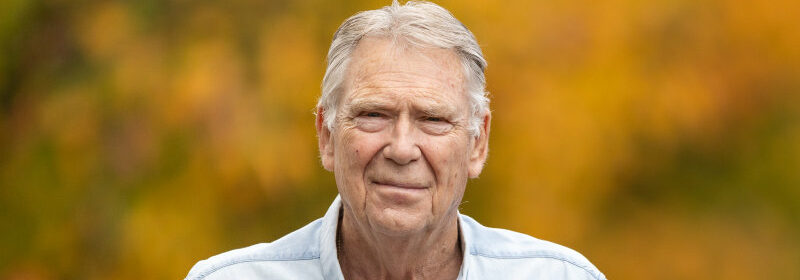
When Rudi De Graaff was diagnosed with diabetes 30 years ago, he didn’t know anyone with the disease.
Now, the Melton local estimates that 40 per cent of the residents living in his retirement village have the health condition.
Rudi De Graaff was diagnosed with diabetes 30 years ago.Credit: Jason South
“It’s concerning,” the 78-year-old said. “People take it for granted, but it could affect their lives in the long run. Your lifespan can be shorter, there can be health complications.”
An analysis of census data as part of this masthead’s State of our Health series shows that Melton, on Melbourne’s western fringe, has the city’s highest rate of diabetes, with 8.2 per cent of residents reporting that they have the disease, compared to a statewide average of 4.7 per cent.
Rich and poor divide
The data does not distinguish between type 1 diabetes, which has a strong genetic link and cannot be prevented, and type 2 diabetes, which people of some ethnicities are more predisposed to, and is linked to being overweight and inactive. About 90 per cent of Australians who have diabetes—which is a group of diseases that cause too much sugar in the blood—have the second variety.
The prevalence of type 2 diabetes is inextricably linked to social disadvantage.
Some of Victoria’s most affluent, inner-city suburbs have the lowest rates of diabetes – the CBD, Port Melbourne, Southbank, West Melbourne, South Yarra and Elwood. Towns and suburbs with higher rates of disadvantage, such as Norlane, Thomastown and Moe, have higher rates of diabetes.
Professor Elif Ekinci, director of the Australian Centre for Accelerating Diabetes Innovations at the University of Melbourne, said people with lower incomes, less knowledge about healthier food options and less time to do physical activity, could be at higher risk of developing type 2 diabetes.
“If you are struggling financially and don’t have the time to feed a family, then processed foods can be the cheaper option,” she said.
Access to sporting facilities, public transport and cycling lanes, are also important, according to Ekinci.
“We need to be doing more in our town planning to prevent diabetes,” she said. “This means having spaces where people can walk rather than relying on their car. That incidental exercise is really important.”
Unhealthy food options
De Graaf believes that the modernisation of Melton has fuelled the spread of the disease.
When he moved to the area in 1985, there were just 16,000 residents and one takeaway option: fish and chips. Now there are 200,000 residents and a smorgasbord of fast food outlets.
“There are big supermarkets and fast food outlets left, right and centre,” the Dutch-born resident says. “These business are looking at places where they can sell their products.”
De Graaf attributes his diagnosis to a poor diet. The aircraft engineer spent decades working shifts at Melbourne Airport and would often eat fatty takeaway meals at all hours of the day. He’d also swig bottles of raspberry soda at home. His excessive thirst and consumption of these sugary drinks prompted his concerned family to ask him to get tested for diabetes.
Cindy Needham, a research fellow at the Global Centre for Preventative Health and Nutrition at Deakin University, has mapped out the distribution of healthy and unhealthy food outlets across Victoria.
She says while most local government areas have the same number of fast food outlets per 10,000 people, ratios of ‘unhealthy’ to ‘healthy’ outlets were highest in growth corridor areas such as Melton.
Residents in these areas have to walk or drive past about nine unhealthy outlets before they find one healthy outlet. In inner-city Melbourne, they have to pass six unhealthy outlets before they reach a healthy outlet.
“In some of the growth areas, what you’ll see is that a supermarket will be put in, and then around that supermarket you’ll have a McDonald’s, a Hungry Jack’s, Red Rooster and 7-Eleven,” she says.
“In some areas you have paddocks and a McDonald’s and a 7-Eleven already built, and the houses hadn’t even come yet.”
She pointed out that having to drive to the supermarket meant that people purchased more unhealthy, non-perishable items and less fresh food because they wanted to avoid frequent trips.
Lifestyle changes
While it is very hard to reverse type 2 diabetes, sufferers can change their lifestyle to manage the disease. This can help prevent diabetes-related complications such as heart attacks, stroke and reduced blood flow to the lower limbs which can lead to ulcers, infections and a heightened risk of amputation.
“People with diabetes can live a really long, healthy life, but it certainly requires effort,” explains Diabetes Victoria’s nurse education team leader Michelle Cox.
Cox says these lifestyle changes mainly involve losing weight and exercising more, but points out that this is not possible for everyone.
Walking is a great way to improve our health.Credit: iStock
“We want to step away from making people with type 2 diabetes feel guilty about having diabetes,” she says.
“If someone has a stigma or shame about an issue, they are less likely to reach out for assistance to help the condition.”
De Graaf made significant changes to his lifestyle following his diabetes diagnosis and has lost 30 kilograms in the process.
He now walks for 30 minutes a day, has swapped frequent beers with a weekly glass of wine, and steers clear of processed foods. He eats plenty of fish, rice and vegetables and takes daily medication to control his insulin levels. He also runs a monthly support session with 20 other residents who live in his lifestyle village and also have diabetes. A diabetes educator from Melton Health has joined the group, and they share recipes and tips on managing the disease.
“If I hadn’t made these changes, my life would have been worse,” De Graaf says.
The Morning Edition newsletter is our guide to the day’s most important and interesting stories, analysis and insights. Sign up here.

